Friday, April 4, 2014
Factors affecting the depth of the burn………
Doc, besides actually looking and evaluating the burn area is there other
ways of knowing that the burn area might be deep?
Marjorie A, Sidney, Australia
A
number of factors should be considered while evaluating the burn depth- temperature
at which the burn is caused, duration of contact, cause of burn and site of
burn.
The
area which is burnt is also important as the skin thickness varies at different
sites (from 1 mm in the genitalia and eyelids to 5 mm in palms and soles). The skin is relatively thinner in children and
geriatric patients and therefore they tend to suffer a greater degree of burns.
Contact
burns tend to be deeper since the burning object or the hot object like the exhaust
of a motorcycle remains in direct contact and causes more damage to the skin.
It must be noted that the lesser the duration
of the burn, the lesser the degree of burn. Therefore it is recommended that
the burn area be cooled at the earliest. Pouring cold water over burns areas
works on this principle and one must within seconds carry out this maneuver to
avoid severe burns. The home kitchen is one area where burns often occur. Fortunately
water is always available in the kitchen and therefore quickly pouring cold or
tap water over the burn area works wonders and one should let the cold water
run over the burn area for a few minutes.
Application
of oil or mint preparations as is often done by lay people should be avoided as
oil stops the heat loss from the surface causing more damage and mint just
gives cools the mind and not the burn area.
The
cause of the burn should be inquired into as different modes of burns can cause
different depths of burns. For e.g. hot water burns are less deep than hot frying
pan oils, as the temperatures of hot oil touch 175-200 degrees compared to hot
water which may be 75-100 degrees. Different acids and bases can cause
different degree of burns depending on their strengths. Thus knowing the burn agent helps a lot in deciding the depth of the burn and predicting the outcome.
We shall discuss how the monitor burn patients in our next post....
(An original initiative in burn care and education from asktheburnsurgeon++)
Thursday, April 3, 2014
Resuscitation Fluids and formulae……….
Doc, how much fluids should be given to a burn patient and
can a person survive if fluids are given if the patient comes to the hospital
many hours after the burn incident?
Shawn, California
As we discussed in an earlier
post, burn wounds loose body fluids from the wound surface as the skin
integrity is damaged. Greater the surface area of the burn, more the fluid
loss. In general the body is able to tackle the fluid loss that occurs from a
less than 15 percent TBSA (total burn surface area) in an adult, and less than 10 percent TBSA in a
child. Beyond this the body’s internal mechanisms are unable to handle this
loss and the patient will end up in shock if the lost body fluids are not
replaced. Once we understand this concept then we are faced with two questions:
a) At what rate should we
administer the intravenous fluids?
b) What is the type of
fluid that we should administer?
Parkland formula
Charles Baxter from parkland hospital
(Texas, USA) made a large contribution to the management
of burns by his studies on the fluid loss in burns and their replacement. He observed
that the first 24 hours were critical to the survival of burn patients and the replacement
of fluids was to be done in the first 24 hours itself. In this the first 8
hours were crucial as the blood vessels and capillaries lost their integrity
totally and therefore the intravascular fluids leaked out on a large scale. In the
second 8 hours after the burn the capillaries regained their integrity and the
leaks were controlled to a great extent. Keeping this in mind Charles Baxter suggested
a fluid resuscitation formula in burn patients at 4 ml/kg/TBSA for the first 24
hours. The type of fluid suggested was Ringer Lactate. Of the total fluid calculated for 24 hours,
half of the volume was to be given in the first 8 hours and the rest in the
next sixteen hours.
Why did Baxter suggest Ringer Lactate
as the resuscitation fluid?
Obviously because he observed that it was more
physiological and had many advantages:
a) Ringer lactate has a lower sodium
concentration (130mEq/L) than normal saline. b)The metabolized lactate had a buffering effect on associated metabolic acidosis in burns.
c)Ringer lactate is an Isotonic crystalloid solution
Example for fluid calculation:
Let’s take an example here – a patient
with a body weight of 65 kg comes to the
ER with flame burns of 45 percent TBSA.
TBSA 45%
Weight of the patient- 65 kg
Therefore the fluid calculation by
parkland formula-
4x% TBSA x body weight
i.e. 4 x 45 x 65
i.e. 11,700 ml for 24 hours
Half of this has to be given in the
first 8 hours
i.e. half of 11,700 – which is 5850
ml for 8 hours
Therefore for each hour in the first
8 hours the patient needs 5850/8 ie 731.25 ml or approximately 730ml per hour
For the next 16 hours the remaining
11700 ml needs to be spread out
So 5850/16 is 365 ml needs to be
given each hour for the next 16 hours
Thus the patient must receive 730 ml
per hour for the first 8 hours post burn and for the remaining 16 hours of the
first day the patient must receive 365 ml per hour.
Coming to the second part of the question- the fluid calculated has to be replaced in the time specified. However some patients appear later than the time of the burn and therefore the fluids which were not administered will have to be replaced at a higher rate but taking care to see that we do not overload the patient and put him into cardiac failure or pulmonary edema.
It must be noted that the calculation
of fluids by this formula is only a guide line and a number of factors must be
taken into consideration which administering fluids which we shall discuss in
another post …..
(An original initiative in burn care and education from asktheburnsurgeon++)
Wednesday, April 2, 2014
Classification of burns...........
Doc, are there different ways to
classify burns?
Mrs. Janice Parker. S. Africa.
Yes there are different ways to
classify burns, but the whole purpose is to help in managing them in a better
way. Every burn must be mentioned by its
degree or depth since it lets the surgeon know whether he should manage the
patient conservatively or by surgery. Further classifying burns in major, minor
or moderate helps to decide the level of management that they need. Thus a
third degree burn even if it is one percent TBSA (total burn surface area) cannot be managed
conservatively and will need surgery. Again a 5 percent TBSA can be managed on
an outpatient basis, but a 50 percent TBSA will definitely need inpatient
management.
degree of burns.
Degree of burn
actually tells us about the depth of the burn. The burn depth is classified as
follows.
a) First degree- superficial
burns affecting the epidermis are referred to as first degree burns and are
similar to sunburns.
b) Second degree: both the epidermis and the
superficial layer of the dermis are damaged in second degree burns.
c) Third degree
burns: these burns affect the full thickness skin and often needs surgical
management.
d) Fourth degree
burns: these burns affect the full thickness of the skin and the underlying
structures like nerves, muscles, tendons, vessels and may extend up to the
bone.
We can also classify burns according
to their size:
a)Major Burns: these consist of chemical or high voltage electrical burns, Inhalation
injury, full thickness burns more than 10% TBSA or burns involving more than
25%TBSA.
b) Moderate Burns: these consist of Superficial
or partial thickness burns of trunk, hands, feet, perineum or head involving
15-25% TBSA.
c) Minor Burns: these
consist of Burns not involving the hand, perineum,
feet or head and must be less than 15% TBSA.
(An original initiative in burn care and education from
asktheburnsurgeon+)
Tuesday, April 1, 2014
ASSESSMENT OF BURN SURFACE AREA……
Doc, what happens if I calculate the burn area wrongly? Is it
really important?
Arthur A, Canada
As we have seen in
previous posts the loss of fluid from the skin surface depends on the degree of
burns and the area of the burns. One must evaluate the total burn surface area
(TBSA) to calculate the fluid requirements. There are different methods of
fluid calculation in burns.
a) Rule of nine
The rule of nine works
well in adult patients. In this method the body surface is divided into various
parts measuring in nines.
Rule of nine
Each arm - 9% TBSA
Head - 9% TBSA
Anterior thorax - 18%
TBSA
Posterior thorax - 18%
TBSA
Perineum - 1% TBSA
Each leg - 18% TBSA
Any burn surgeon will tell you that more
often the burns are so irregularly placed that accurate calculation becomes
difficult in different regions of the body. In such cases a simple trick is to
use the palm of the hand as a method of calculation. At any age the palm of the
hand is approximately 1% and can be used to measure the burn areas. One must not forget that it is the patient’s
hand that is used for the calculation and not the doctor’s. An approximate size
of the palm of the patient is considered and the equivalent burn area is
estimated. For e.g. lets say the burn area was 5 palm sizes of the patient over
the body and lower limbs. Now we can assume that the patient has about 5% burns.
It should be noted that first degree
burns do not produce fluid losses and therefore only 2nd degree
burns or more should be used for fluid calculation.
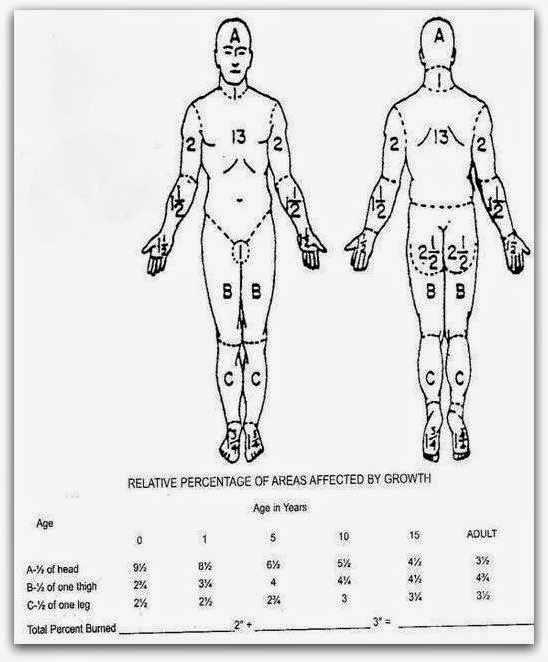
However in children the rule of nine
can lead to serious errors as the head and body is larger in TBSA than the
limbs and therefore the Lund and Browder charts work out to be
more accurate while calculating the fluids to be administered. The Lund and Browder chart is shown below.
If the fluid calculation is wrong
then the patient will be administered less fluids and this will result in shock
or low volume circulatory failure and ultimately may be fatal. The fluids calculated need to be replaced
within a time limit as we shall discuss in the next post. Correct volume replacement
and correct timing is what makes the resuscitation of burns patients
successful.
(an original initiative in burn care and education from
asktheburnsurgeon+)
Sunday, March 30, 2014
How burns affect the tissues.....
Doc, could you please explain the cellular and chemical
processes that occur when the tissues are burnt?
Rony v, Goa
A number of inflammatory processes both local (at the site of
the burn) as well as systemic (in the rest of the body) take place when burns
occur which eventually lead to the shifting of fluid from the vascular
compartment to the interstitial spaces. Subsequent to the burn a number of
cells like Neutrophils,
macrophages, and lymphocytes cross over into the burned tissues and start releasing
chemical mediators like histamine, serotonin, prostaglandins, kinins, platelet
products and complement components. These chemical substances damage the normal
blood capillary barrier which leads to an increase in the permeability of the
vessels. Intravascular fluids therefore start to leak from the walls of the
vessels and this ultimately leads to a decrease of the circulating
intravascular blood volume. A fact that is not commonly recognized is that
these processes that occur in the burn tissues also take place in the tissues
that have not suffered any burns and therefore one can see edema in areas of
the body that have not suffered burns. Thermal injury also ends up damaging the
cell wall and collagen fibers which in turn lead to inadequacy of the cell wall
transport mechanisms and buildup of sodium and water and eventual death of the
cell if the fluid imbalances are not immediately corrected. In minor burns such
as 10 percent in children and about 15 percent in adults these fluid balances
are well adjusted and tolerated and therefore additional fluid replacements are
not needed. However in patients with TBSA higher than the one’s mentioned above
intravenous fluid resuscitation is needed.
The capillaries begin to
regain their functional integrity and the leak eventually gets controlled, but
this often takes more than 8 hours post burn. Crystalloids are usually given in
the first 8 hours and one’s the integrity of the capillary wall is regained
after 8 hours, colloid fluids are started since they will not leak out. Adding
colloids also help to reduce the fluid overload that may result of excess of
crystalloid infusions. Burn wounds are composed of three zones- a central zone
of coagulation or severe tissue damage, a peripheral zone of hyperemia or
vasodilatation, and an intervening zone
of stasis or low blood flow (ischaemia). If the fluid imbalances that occur
from the fluid shifts as noted above are not corrected on time then these zones
can extend and more tissue damage can result explaining the fact that some
superficial burns on admission can end up as deep over period of time. This can
also happen when burn wounds get infected.
(an original initiative in burn care education from asktheburnsurgeon)
+
Subscribe to:
Posts (Atom)